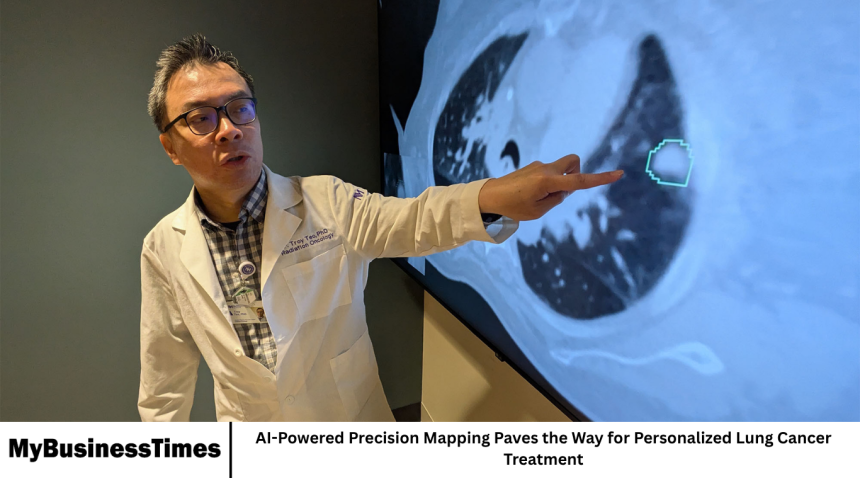
A groundbreaking advancement in medical research is reshaping the future of cancer care. Researchers have developed an artificial intelligence (AI)-powered precision mapping approach that promises to revolutionize the diagnosis and treatment of lung cancer. This new technology uses advanced data analysis and machine learning to map tumors with remarkable accuracy, allowing doctors to design personalized treatment plans for each patient.
Lung cancer remains one of the leading causes of cancer-related deaths worldwide. Despite significant progress in early detection and therapy, many patients are still diagnosed at later stages when treatment options are limited. The introduction of AI-driven precision mapping could be a major step forward in improving survival rates and enhancing quality of care for patients.
Understanding Precision Mapping
Precision mapping refers to the process of creating a highly detailed and individualized profile of a tumor. Using imaging scans, genetic information, and clinical data, AI algorithms analyze the specific characteristics of cancer cells to understand how they grow, spread, and respond to treatment.
Traditional methods rely heavily on visual examination of scans and manual interpretation by medical experts. In contrast, AI-based precision mapping can detect subtle patterns invisible to the human eye, helping doctors identify tumor behavior earlier and more accurately.
This level of detail allows clinicians to tailor treatment plans to each patient’s unique cancer profile rather than using a one-size-fits-all approach.
The Role of Artificial Intelligence
Artificial intelligence plays a central role in this new approach. The technology uses deep learning—a type of machine learning inspired by the structure of the human brain—to process large amounts of medical data quickly and efficiently.
AI algorithms are trained on thousands of lung cancer cases, learning to recognize patterns in imaging scans, pathology slides, and genetic sequences. Once trained, these systems can analyze new patient data to generate precise maps of tumor structure and predict how the disease might progress.
This information helps oncologists decide which therapies are most likely to work for a particular patient, reducing unnecessary treatments and improving overall outcomes.
Benefits for Early Detection
One of the most promising aspects of AI-driven precision mapping is its potential to improve early detection. Lung cancer often develops silently, with symptoms appearing only in later stages. By identifying molecular and structural changes early on, AI can flag potential problems before they become life-threatening.
Researchers say that this technology could lead to faster diagnoses and allow for timely interventions that significantly improve survival rates. Early detection also opens the door for less invasive treatments and reduces the need for aggressive therapies such as chemotherapy and radiation.
Personalized Treatment Planning
Every cancer patient is unique, and so is every tumor. Traditional treatment methods often fail to account for this individuality. With AI-based precision mapping, doctors can design treatment plans tailored specifically to the patient’s biological makeup.
For example, if the AI identifies that a patient’s tumor is more likely to respond to targeted therapy rather than chemotherapy, doctors can adjust the treatment accordingly. This personalized approach helps minimize side effects, lowers treatment costs, and improves the likelihood of success.
In addition, precision mapping can help identify which patients are most likely to benefit from immunotherapy, one of the most advanced forms of cancer treatment available today.
Real-World Applications and Clinical Trials
Hospitals and research institutions around the world are beginning to adopt AI-powered tools in cancer care. Clinical trials are already underway to test the effectiveness of precision mapping in improving diagnostic accuracy and patient survival rates.
Preliminary results show that AI-assisted mapping provides more consistent and objective results than traditional methods. It also reduces the time required for diagnosis, allowing doctors to begin treatment sooner.
In some cases, AI systems have even detected early signs of tumor recurrence before they were visible in standard imaging tests, giving patients a valuable head start in treatment.
Challenges in Implementation
While the potential of AI-powered precision mapping is enormous, several challenges remain before it can be widely adopted.
One of the main hurdles is data availability. AI systems require large, high-quality datasets to train effectively. Differences in medical imaging standards, patient demographics, and health record systems can make it difficult to collect uniform data.
There are also concerns about privacy and data security. Medical data must be handled carefully to ensure patient confidentiality and comply with global data protection laws.
Additionally, integrating AI systems into existing healthcare workflows requires training and collaboration between doctors, researchers, and technology specialists.
Collaboration Between Medicine and Technology
The success of precision mapping depends on strong collaboration between the medical and technology sectors. Hospitals, universities, and tech companies are working together to refine algorithms, improve data sharing, and make AI tools more accessible to clinicians.
Major technology firms are investing heavily in healthcare AI research, while medical institutions are creating dedicated departments focused on digital health and precision medicine. This cross-disciplinary cooperation ensures that innovation continues to progress in a responsible and ethical way.
How AI Transforms Patient Care
AI-powered mapping does more than assist doctors—it transforms the patient experience. Patients benefit from quicker diagnoses, more accurate results, and personalized care plans that consider their unique biology and lifestyle.
With AI providing real-time analysis, doctors can spend more time focusing on communication, counseling, and emotional support, which are essential parts of cancer care.
Moreover, by reducing unnecessary treatments and hospital visits, AI technology can lower healthcare costs and make advanced cancer care more accessible to a wider population.
Ethical Considerations and Data Security
As AI takes a larger role in medicine, ethical concerns are becoming increasingly important. Data privacy, algorithm bias, and accountability are central issues that must be addressed to ensure fairness and transparency.
Developers are now building AI models that comply with strict ethical standards, ensuring that patient data remains confidential and that algorithms produce unbiased results regardless of race, gender, or background.
Healthcare regulators and policy-makers are also working to establish frameworks for approving and monitoring AI-driven medical technologies.
Future Outlook
The use of AI in precision mapping marks a major step toward the future of personalized medicine. Experts believe that within the next decade, AI could become a standard part of cancer diagnosis and treatment planning.
Researchers are already exploring how this approach could be expanded to other forms of cancer, including breast, prostate, and brain tumors. As AI continues to evolve, its integration with genomics, imaging, and clinical data could make medicine more predictive, preventive, and personalized than ever before.
With further development, AI-driven mapping could one day help doctors identify cancer risks before tumors even form, transforming the way healthcare professionals approach prevention and treatment.
The Global Impact of AI in Cancer Care
AI’s potential extends far beyond individual hospitals or countries. It can help bridge healthcare gaps between developed and developing regions by providing diagnostic support in areas where medical specialists are scarce.
Through cloud-based systems, doctors in remote locations can access AI tools to analyze scans and receive expert-level insights within minutes. This could dramatically improve cancer care accessibility and outcomes in underserved regions.
Organizations such as the World Health Organization and global research consortia are supporting efforts to make AI-driven medical tools widely available, ensuring equitable access to technology-based healthcare solutions.
Frequently Asked Questions
What is AI-powered precision mapping in lung cancer treatment?
It is a method that uses artificial intelligence to analyze medical data and create detailed maps of lung tumors, helping doctors design personalized treatment plans.
How does AI improve lung cancer diagnosis?
AI can detect subtle patterns in scans and data that humans may miss, enabling earlier and more accurate diagnosis of lung cancer.
Is this technology already in use?
Yes, AI-driven precision mapping is being tested in hospitals and research centers worldwide, with promising results from early clinical trials.
What are the benefits for patients?
Patients receive faster diagnoses, more targeted treatments, fewer side effects, and a greater chance of recovery thanks to personalized care plans.
What challenges does AI face in healthcare?
Key challenges include data privacy, standardization, and integration into existing healthcare systems, as well as ensuring ethical use of patient information.
Could this approach help treat other cancers?
Yes, researchers believe AI precision mapping could be applied to other cancers such as breast, prostate, and brain cancer to enhance diagnosis and treatment.
Conclusion
AI-powered precision mapping represents a new era in lung cancer diagnosis and treatment. By combining advanced data analytics, machine learning, and clinical expertise, this technology enables doctors to understand tumors with unprecedented precision.
While challenges remain in terms of data sharing, ethics, and integration, the progress so far offers hope for millions of patients around the world. With continued collaboration between scientists, doctors, and technology developers, AI-driven precision mapping may soon become a cornerstone of modern cancer care.